Case of the Month Jan 2011
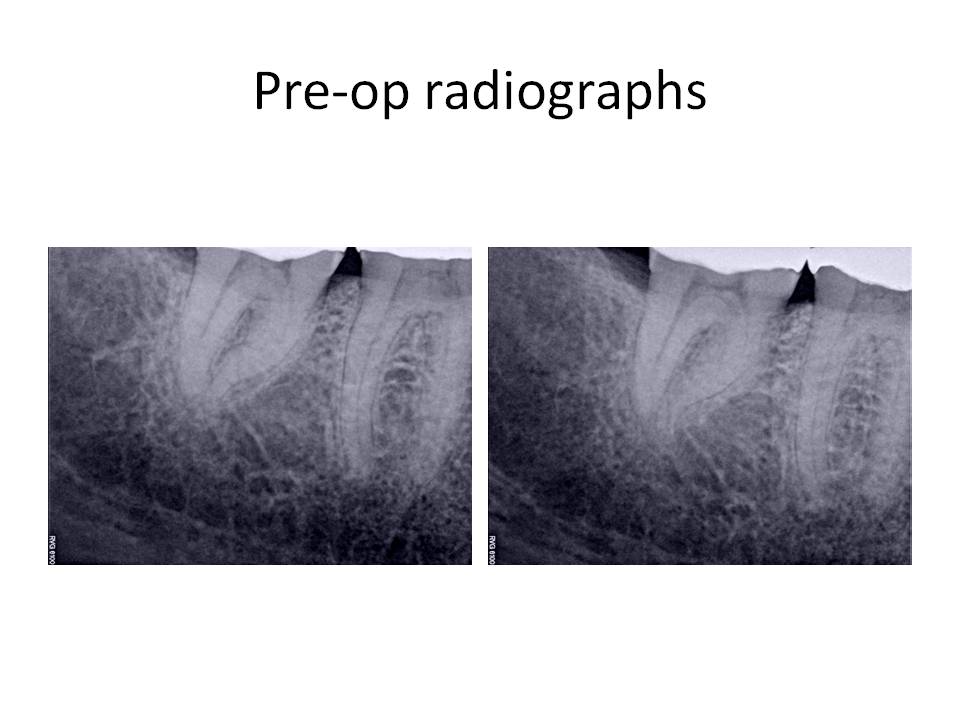
Happy New Year to all of you! This month, I am presenting a case of a severely dilacerated meisal root on tooth #31. The patient presented with CC of sensitivity to cold ever since she had a crown placed on the tooth. She had cracked the tooth or exisiting restoration that was present, and therefore, required a crown on the tooth. The patient had increasing sensitivity to cold over the past 3 months. Clinical exam revealed a FGC tooth #31, hyperreactive to cold that was more pronounced and lingered significantly more than the adjacent teeth, slight percussion tenderness, normal periodontal probing depths. Radiographs revealed a S-shaped mesial root #31 with no periradicular pathosis visible. Her medical history had positive entries for ovarian cancer 10 years ago and PCN causing nausea, but otherwise unremarkable. Here are the pre-operative radiographs. 
The clinical diagnosis was Irreversible pulpitis #31 with symptomatic periradicular periodontitis. The informed consent was signed and administration of local anesthetic was given. After several injections, the patient was still unable to achieve profound anesthesia. I had used 1 carpule of each anesthetic to attempt to adequately numb the area ( 2% Lidocaine with 1:100,000 epi, 3% Mepivicaine, 0.5% Marcaine with 1:200,000 epi, 4% Articaine with 1:100,000 epi). She was given an IAN block, a Gow-Gates, PDL, Buccal Nerve and Lingual Nerve, and an infiltration injection. The endodontic treatment was not attempted, due to lack of profound anesthesia. The patient was dismissed and I recommended that she take 3, 200mg Advil Liquigels 30 minutes prior to her next appointment to help with the anesthesia. There is a paper by Dr. Ken Hargreaves that discusses the use of local anesthetics and how the pH is affected by increasing amounts of epinephrine and why different anesthtic types without epi can be beneficial in these situations. Also, he talks about the need to close the TTX channels with the administration of an NSAID that are typically resistant to local anesthetics.
At the next appointment, the same types of anesthetics were given as noted previously, with two exceptions to the first appointment. First, the patient had taken the Advil as directed and second, I gave her a closed mouth injection known as the Akinosi technique of local anesthetic administration. She obtained profound anesthesia and I was able to perform the root canal treatment as planned. Post-op radiographs:

The final radiograph demonstrated two distal canals, one of which (DL), exited very short of the other. I welcome any comments or questions. Thank you for your continued confidence in my practice.
The clinical diagnosis was Irreversible pulpitis #31 with symptomatic periradicular periodontitis. The informed consent was signed and administration of local anesthetic was given. After several injections, the patient was still unable to achieve profound anesthesia. I had used 1 carpule of each anesthetic to attempt to adequately numb the area ( 2% Lidocaine with 1:100,000 epi, 3% Mepivicaine, 0.5% Marcaine with 1:200,000 epi, 4% Articaine with 1:100,000 epi). She was given an IAN block, a Gow-Gates, PDL, Buccal Nerve and Lingual Nerve, and an infiltration injection. The endodontic treatment was not attempted, due to lack of profound anesthesia. The patient was dismissed and I recommended that she take 3, 200mg Advil Liquigels 30 minutes prior to her next appointment to help with the anesthesia. There is a paper by Dr. Ken Hargreaves that discusses the use of local anesthetics and how the pH is affected by increasing amounts of epinephrine and why different anesthtic types without epi can be beneficial in these situations. Also, he talks about the need to close the TTX channels with the administration of an NSAID that are typically resistant to local anesthetics.
At the next appointment, the same types of anesthetics were given as noted previously, with two exceptions to the first appointment. First, the patient had taken the Advil as directed and second, I gave her a closed mouth injection known as the Akinosi technique of local anesthetic administration. She obtained profound anesthesia and I was able to perform the root canal treatment as planned. Post-op radiographs:
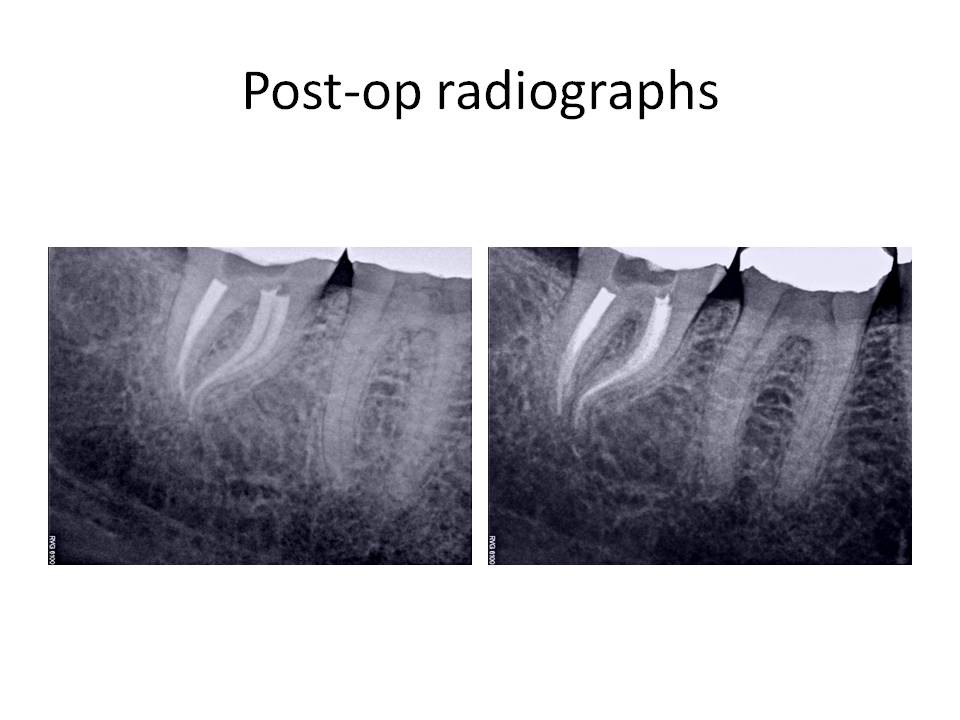
The final radiograph demonstrated two distal canals, one of which (DL), exited very short of the other. I welcome any comments or questions. Thank you for your continued confidence in my practice.