Case of the Month September 2010
This month I will present a case in which removal of a separated instrument was performed.
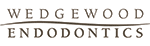
The patient is a 41 y.o. male who presented with the chief complaint of swelling and pain associated with tooth #30. His medical history revealed a positive entry for high blood pressure which was well-controlled with Amlodipine and for tobacco use. His dental history associated with tooth #30 was as follows. He had pain approximately 1 year ago and had root canal therapy performed. At the time of the treatment, the patient was informed of a separated instrument in one canal and assured that the tooth would be fine. Treatment was completed and a crn was placed on the tooth. Approximately 2 weeks before he presented to my office, he experienced swelling on the right side of his mandible. He was being treated for a sinus infection at the same time and was taking antibiotics. He noted that the swelling had resolved and his pain was also reduced. Clinical exam #30 reveals PFM crn present, perio pocketing was noted DL and DB of 5-6mm, tenderness to percussion and expansion of the buccal cortical plate was noted. Radiographically, RCT was done and the tooth was instrumented and obturated well short of the radiographic apex in all canals, RL lesion was associated with the Distal root, and a separated file was present mid-root in the MB canal. The crn also appears to be ill-fitting with an open mesial margin.

The clinical diagnosis is Previously treated #30 with symptomatic periradicular pedoni. The recommended treatment was non-surgical retreatment with the added provision that the removal of the separated instrument will be attempted in order to completely instrument the canals. The goal of the first appointment was to remove the previous obturation material and begin the instrument removal process. After removal of the Gutta Percha, calcium hydroxide was placed as an interim medicament. The second appointment consisted of continuing the attempt at removal of the instrument, but to no avail. However, the canals that were accessable, were cleaned and shaped to length. The ML canal was blocked and had to be negotiated to length. At the third appointment, the instrument was finally loosened and removed form the tooth.
The case was finished and the patient was instructed that a new crn was indicated due to the open mesial margin.
The difficulties in this case were two-fold. First, the canals that were instrumented were blocked and inadequately cleaned and shaped. The second problem was of course the separated instrument. The removal of broken files is dependent on several factors: 1. Location – the higher up in the root, the liklihood of removal is increased, 2. If the fragment is not around a bend which would restrict straight-line visualization of the instrument and 3. The amount of root structure that would remain after instrument removal. The technique involves the use of ultrasonic tips, platforming to visualize the instrument, the use of a surgical operating microscope and finally, and most importantly, PATIENCE!
I welcome all comments or questions. Thank you for continuing to trust in our practice. We wish to be your first choice in endodontic care for your patients.
The patient is a 41 y.o. male who presented with the chief complaint of swelling and pain associated with tooth #30. His medical history revealed a positive entry for high blood pressure which was well-controlled with Amlodipine and for tobacco use. His dental history associated with tooth #30 was as follows. He had pain approximately 1 year ago and had root canal therapy performed. At the time of the treatment, the patient was informed of a separated instrument in one canal and assured that the tooth would be fine. Treatment was completed and a crn was placed on the tooth. Approximately 2 weeks before he presented to my office, he experienced swelling on the right side of his mandible. He was being treated for a sinus infection at the same time and was taking antibiotics. He noted that the swelling had resolved and his pain was also reduced. Clinical exam #30 reveals PFM crn present, perio pocketing was noted DL and DB of 5-6mm, tenderness to percussion and expansion of the buccal cortical plate was noted. Radiographically, RCT was done and the tooth was instrumented and obturated well short of the radiographic apex in all canals, RL lesion was associated with the Distal root, and a separated file was present mid-root in the MB canal. The crn also appears to be ill-fitting with an open mesial margin.
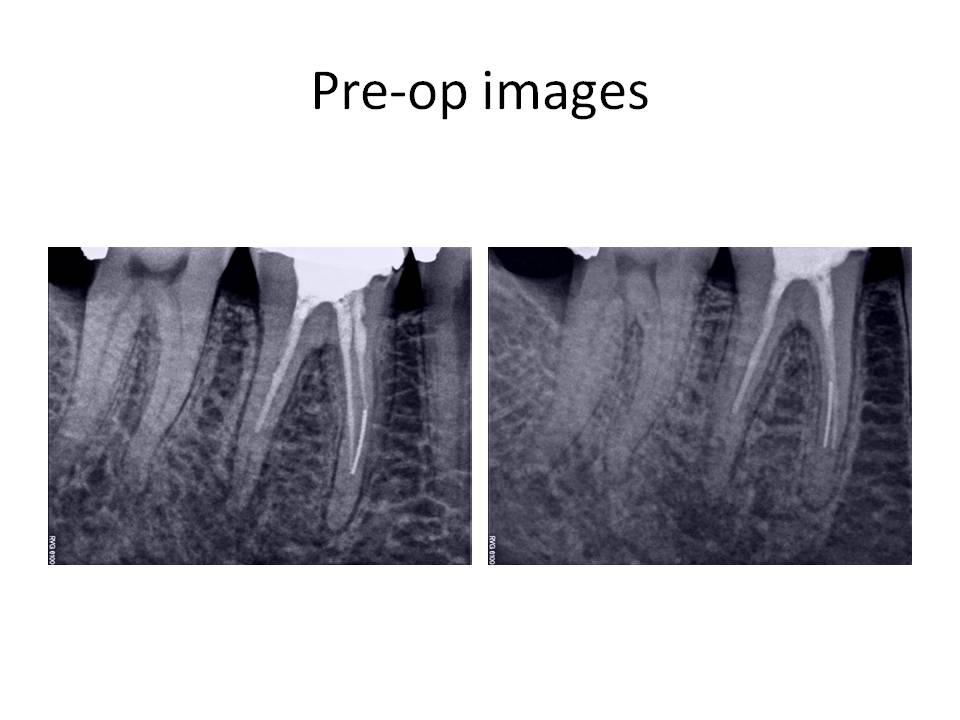
The clinical diagnosis is Previously treated #30 with symptomatic periradicular pedoni. The recommended treatment was non-surgical retreatment with the added provision that the removal of the separated instrument will be attempted in order to completely instrument the canals. The goal of the first appointment was to remove the previous obturation material and begin the instrument removal process. After removal of the Gutta Percha, calcium hydroxide was placed as an interim medicament. The second appointment consisted of continuing the attempt at removal of the instrument, but to no avail. However, the canals that were accessable, were cleaned and shaped to length. The ML canal was blocked and had to be negotiated to length. At the third appointment, the instrument was finally loosened and removed form the tooth.
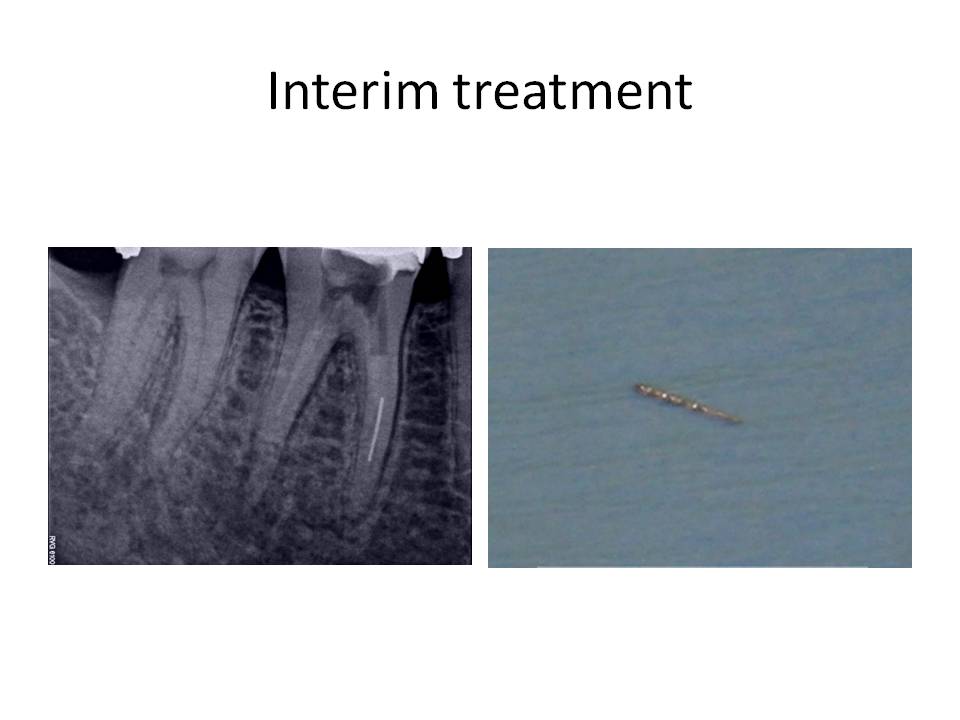
The case was finished and the patient was instructed that a new crn was indicated due to the open mesial margin.
The difficulties in this case were two-fold. First, the canals that were instrumented were blocked and inadequately cleaned and shaped. The second problem was of course the separated instrument. The removal of broken files is dependent on several factors: 1. Location – the higher up in the root, the liklihood of removal is increased, 2. If the fragment is not around a bend which would restrict straight-line visualization of the instrument and 3. The amount of root structure that would remain after instrument removal. The technique involves the use of ultrasonic tips, platforming to visualize the instrument, the use of a surgical operating microscope and finally, and most importantly, PATIENCE!
I welcome all comments or questions. Thank you for continuing to trust in our practice. We wish to be your first choice in endodontic care for your patients.