June 2017
Patient is a 41 year old Caucasian female who presented with the Chief complaint of sudden pain on the left side of her face and dentition for the past 2 days. Her medical history is unremarkable with the only medication she is currently taking is Ibuprofen for the control of her sudden onset of pain. The patient was seen by her dentist and referred for evaluation of tooth #19 due to radiographic apical pathology.
Clinically, tooth #19 has an MOD composite restoration with good margins, normal (similar to adjacent teeth) response to cold, negative percussion tenderness, slight palpation tenderness and very mild cortical plate expansion near the distal root end, normal periodontal probing depths, no mobility noted. Radiographs reveal conservative composite restoration present, a circular RL lesion (12 x 12 mm) associated with the distal root end. The outer 2-3 mm circumference of the lesion appears more radiodense while the center appears more lucent and has an irregular trabecular pattern.
External palpation of the left Masseter and Temporalis muscles produces some mild discomfort. From the clinical and radiographic exam, I will aske the question as to whether this is a LEO(Lesion of Endodontic Origin) or non–LEO?
I present the radiographs for this case.
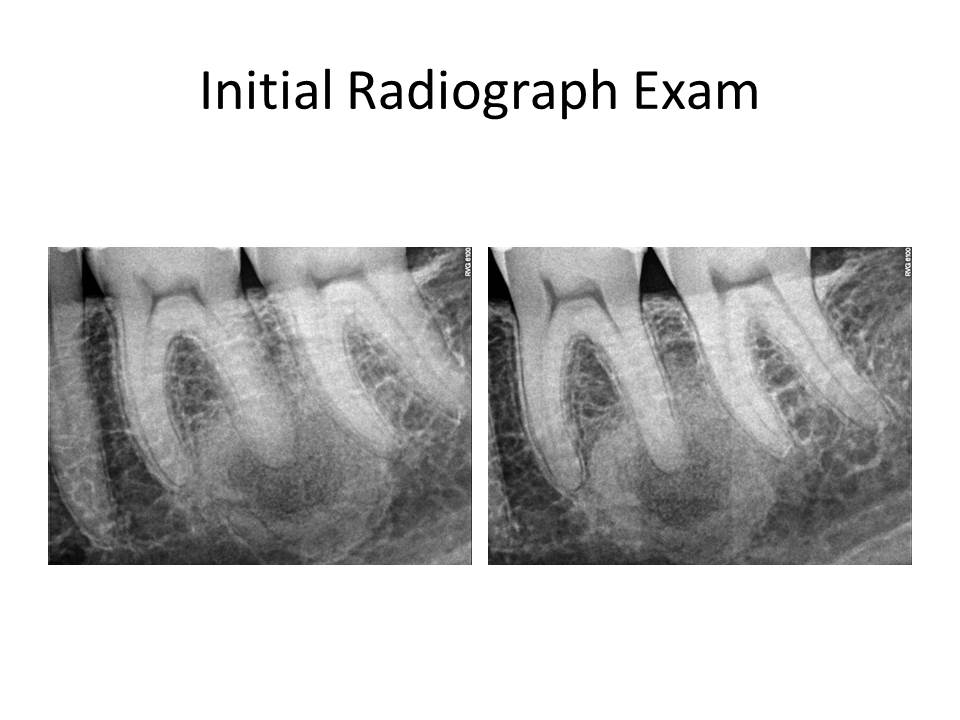
Since the tooth responded similarly to cold as the adjacent teeth and the restorative treatment was conservative, I initially did not think this was an endodontic issue. The pain the patient was reporting as sudden onset was actually related to nocturnal bruxism and stress as she was getting married in a few days. So, I have ruled out root canal treatment. What is the differential diagnosis? What are the potential treatment options for this case, if any?
My differential diagnosis included the following:
1. Ossifying Fibroma (early stage)
2. Focal cemento-osseous dysplasia
3. Simple bone cyst
4. Ameloblastoma
5. Keratocystic odontogenic tumor
The diagnosis is #2. Focal cemento-osseous dysplasia. Review of the patient’s pano did not reveal any other locale for additional pathosis. If so, this would be a case of Florid cemento-osseous dysplasia. Treatment is observation, unless the lesion becomes large enough to cause discomfort. In which case, enucleation of the lesion would be indicated. These lesions become problematic when they become large and communicate with the oral cavity. Also, hypovascularization can occur and these lesions can be prone to necrosis with minimal provocation. At this time, annual radiographic examination is the only treatment recommended.
Thank you for the opportunity to serve your practice and patient’s needs!